NEWSLETTER
Osteoarthritis & osteoporosis common in women
Don’t neglect your bone health!
Typically male, typically female? Depression and eating disorders, as well as osteoporosis, affect women much more frequently. Hormones are to blame – but so is age.
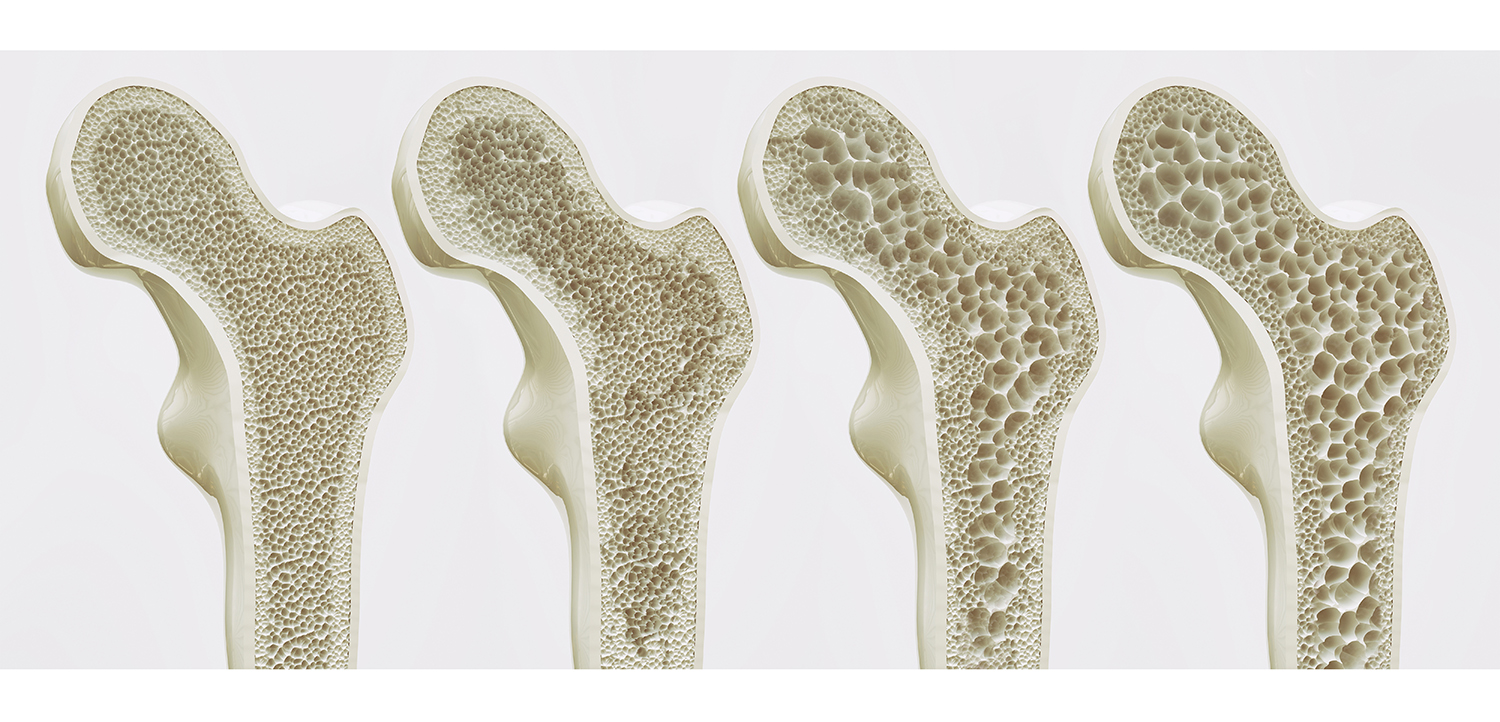
Age also affects bones
Osteoporosis: women particularly at risk
Women suffer from musculoskeletal disorders such as osteoarthritis or rheumatoid arthritis more frequently than the “stronger” sex. Reason enough to take a closer look at osteoporosis as an example.
There are several reasons why women fall ill more frequently:
- In adults, the sex hormones maintain the balance between osteoclasts, which break down bone, and osteoblasts, which build bone. After the menopause, oestrogen levels drop significantly. The result: physiologically, bone density decreases by up to 2% per year, especially at the beginning of the menopause!
- Women have a lower bone mass overall
- On average, women live 4.8 years longer than men. The risk of osteoporosis increases with age. While only around 15% are affected between the ages of 50 and 60, the prevalence rises to 45% over the age of 70
- Women generally consume less Calcium through their diet. Pregnancy and breastfeeding can also increase the need for Calcium and other nutrients.
![Knochenumbau_365865351 [Konvertiert]](https://www.kyberg-vital.de/wp-content/uploads/2023/06/Knochenumbau_365865351-Konvertiert.png)
Prevention is essential
Perfect duo: Magnesium and Calcium
Unfortunately, only about one third of the Calcium in food can be utilized. After being released from food by digestive juices, Calcium is actively absorbed in the duodenum and proximal jejunum. It is regulated by the active vitamin D hormone and the parathyroid hormone, so that an adequate vitamin D level is essential. Although passive absorption is also possible at high doses, Calcium is best absorbed throughout the day. In order for it to be optimally utilized, a single dose should not exceed 500 mg.
Calcium carbonate is difficult to absorb. This is particularly true if you are taking proton pump inhibitors or in older patients, as their gastric acid secretion often decreases. Organically bound Calcium salts such as Calcium citrate, Calcium gluconate or Calcium lactate are a better alternative. The combination with the amino acid lysine also increases calcium absorption. Micronutrient deficiencies (vitamin B6, iron, Zinc), on the other hand, can interfere with calcium absorption and/or utilization.
Magnesium and Calcium are both preferentially absorbed in the small intestine, but do not inhibit each other. Quite the opposite! A prolonged magnesium deficiency even leads to a calcium deficiency, which cannot be corrected by an increased calcium intake.
Our tip: An elevated homocysteine level has been shown in epidemiological studies to be a risk factor for bone fractures in osteoporosis. The level can be favorably influenced by a targeted intake of folic acid and vitamin B12. However, due to a lack of data, the S3 guideline on osteoporosis has not yet been able to come up with a general recommendation for supplementation or measurement. This expired in 2022 and is currently being revised.







